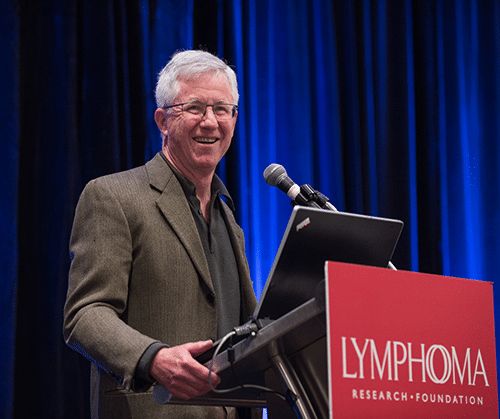
Geoff, Chronic Lymphocytic Leukemia Survivor
Geoff, Chronic Lymphocytic Leukemia Survivor

I recently marked my tenth anniversary as a lymphoma survivor. After a complex and sometimes scary course of my cancer, I’m in remission. I feel great and am incredibly thankful for the advances in blood cancer research that helped get me here. I’m a very happy man.
In the Fall of 2009, I was happy, too. I was in great shape, eating right, and felt like a million bucks. Then a routine physical changed everything.
My primary care provider called me and said, “Your white blood cell numbers have been rising steadily. They are now out of range and still rising. You need to see a hematologist/oncologist and do it soon.” I was totally shocked and angry at the very unsettling news.
An oncologist soon confirmed I had chronic lymphocytic leukemia (CLL). I had never heard of it.
I knew I needed solid information and wanted it fast. I quickly discovered the Lymphoma Research Foundation. All the reliable information on their site about my disease gave me clarity and helped calm me down.
Most importantly, I learned that my kind of lymphoma, while incurable and sometimes deadly, is often slow-paced. Many people do not need treatment and patients and can live long and full lives.
My next step was finding a lymphoma specialist experienced in CLL who I could trust and who would come up with the best treatment plan for me. I found Foundation’s former Scientific Advisory Board member, Dr. Bruce Cheson, MD. He said my cancer was progressing, but slowly. He explained that the toxicities of early intervention far outweighed any possible benefits and recommended active surveillance (watch and wait).

Although living with uncertainty wasn’t easy, for the next five years I lived my life fully, much as I always had. And during those five years, the science developed very quickly. Entirely new understandings and new therapies emerged. It was a very exciting time with lots of hope.
By early 2015, my CLL was advancing fast. I felt terrible: severe and rapid weight loss, extreme weakness and fatigue, appetite loss, and an enlarged spleen. My white blood cell counts were escalating very rapidly. Treatment time had arrived.
After speaking with Dr. Cheson, I decided to enroll in a clinical trial as my first form of treatment. I’m a huge believer in clinical trials. Without them, the science can’t be tested, and new treatments and drugs can’t get FDA approval. Plus, trials often provide access to new therapies that aren’t available anywhere else.
I received intravenous chemotherapy and immunotherapy with the drugs bendamustine and rituximab, plus an emerging targeted agent called idelalisib that’s taken as a pill. My body could not tolerate the new targeted agent, so I had to stop taking it. However, the chemoimmunotherapy worked and helped me achieve a partial remission.
Unfortunately, my partial remission only lasted a little over a year, until my blood numbers began rising quickly again. However, Dr. Cheson felt that was not ready to start treatment again since I felt fine and major symptoms had not yet appeared.
But then one day in 2017, I began to lose vision. Within two weeks I had lost all sight in one eye and partially lost it in the other. Retina specialists determined that my lymphoma had spread outside the lymphatic system and had invaded my retinas and optic nerves.
Soon after losing my vision, I started having frequent seizures involving the entire left side of my body.
Dr. Cheson ordered a spinal tap, an MRI, and additional tests. He found that my CLL had in fact spread to my eyes, brain lining, and central nervous system. This spread is extremely rare for CLL; I’m told that only one other case besides mine has ever been recorded.
Due to the rarity of this presentation, there is no standard of care. Dr. Cheson had to invent one. He consulted other experts and recommended high-dose chemotherapy for my brain lining and central nervous system, infused through a spinal tap. We used high doses of a drug called cytarabine that’s often used for brain cancer.
In addition, Dr. Cheson prescribed high doses of ibrutinib, a newer targeted agent taken orally. The Ibrutinib was able to cross the blood-brain barrier to reach my brain and central nervous system and do its magic.
This novel combination treatment worked, thankfully. My vision returned, the seizures stopped, and it beat back the CLL again. I have been in full remission for over two years.
Once again, on my tenth anniversary since diagnosis, I am fit, feeling great, and a happy man.
None of this would have been possible without all the amazing advances in blood cancer research over the past ten years. For example, the maintenance drug I’m now on, acalabrutinib, did not exist when I was diagnosed in 2009. My brand-new drug and others like it use sophisticated mechanisms that were not well understood back then. Now many of these new drugs are helping patients to stay alive and to feel great.
After a long ten-year journey, I no longer fear my lymphoma! I trust my specialist and I trust the science that underpins the rapidly advancing research. I have very high hopes for me and all of my fellow blood cancer survivors. I’m especially grateful for all the support that the Lymphoma Research Foundation has given to help speed the research and to support the lymphoma community.