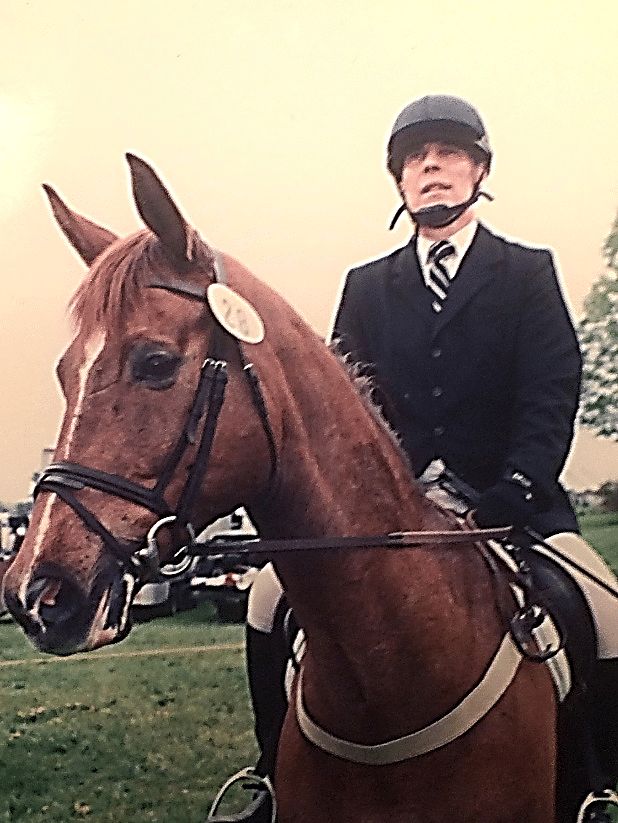
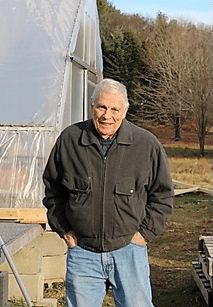
Gil, B-Cell Lymphoma Survivor
Gil, B-Cell Lymphoma Survivor
I was sitting alone in a stark, clean examination room on September 16, 2021, at the Dana Farber Cancer Institute (DFCI) in Brookline, Massachusetts, my son and spouse listening in on my cell phone, when my oncologist walked in.

My doctor said that this morning’s PET-CT scan showed that an area above my sinuses had grown some compared to the scan three months ago, as well as a small new spot that was lit up on my liver. A recent biopsy of a polyp on the roof of my mouth had also — based on extensive cellular analysis — shown recurrence of cancer with the CD20 protein. (Remember this – we’ll come back to it in a few minutes.) It looked like this was a relapse from previous treatments for a fast-growing B-cell lymphoma and should be addressed.
I asked, “What are the options for future treatments?”. She said that the standard of care for my situation and at the age of eighty was another combination of chemo drugs called PBN (polatuzumab vedotin, bendamustine, and rituximab) over six cycles that could start immediately. Stem-cell transplant was out of the question because of my age, and the previous treatments would probably not work.
I asked what was my prognosis? Her response was a shock: “Maybe 12 to 24 months.” The cure rate was only 30%, meaning that there was 70% probability it could relapse.
This was the offered “next step” in my treatment.
I asked if she knew about “Mosun” or “mosa,” or “something like that?”. She responded that yes, DFCI had been involved in clinical tests of this new drug (mosunetuzumab) some time ago, but they were not involved with it now. The FDA hadn’t approved it yet. Further, she said there were no clinical trials available for me.
My drive home while talking to my wife was discouraging – I had basically received a death sentence on my life in the very near future.
This all began in 2006 when I noticed that my platelet count appeared to be falling steadily from year to year. An engineer by training, I had developed graphs of several of my key blood counts for years such as red count, white count, hematocrit, hemoglobin, and platelets. If you only looked at the blood counts on that day you wouldn’t really see much of a problem – maybe some of the measurements were a little low.
But when the graph showed my platelet count dropping down to less than 50 K/μL, my PCP recommended that I see a hematologist/oncologist at Newton-Wellesley Hospital.
This specialist suggested I immediately have a bone-marrow biopsy, which showed that I had a slow-growing type of non-Hodgkin lymphoma. Basically, the lymphoma in my bone marrow was crowding out production of other cells; red blood cell counts, for example, were starting to fall and I was getting anemic, even passing out occasionally.
My doctor, a Boston-area leading expert on B cell non-Hodgkin lymphoma and a senior doctor at DFCI, first started me in 2006 on a regimen of rituximab. When this wasn’t totally effective, we then tried 5 cycles of fludarabine and rituximab starting in 2009. The disease disappeared until 2015 — almost six years in remission. However, it reoccurred and in October 2015, I began five cycles of R-CHOP, the strong cocktail of chemo drugs traditionally infused for non-Hodgkin’s lymphoma patients. This was also effective until late in 2020 when nasal and sinus problems started to appear. After PET-CT scans and a nasal biopsy were performed it revealed that the lymphoma had come back in a somewhat transformed state.
Around Christmas in 2020, I began CAR-T therapy at Brigham & Women’s Hospital. I felt fortunate to avoid any of the severe side effects that can come along with CAR-T, though I was briefly hospitalized for the re-transfusion.
This worked for about nine months and my most recent tests and scans showed no cancerous CD19 B cells in my blood (success!). However, cancerous lymphoma was still growing but differently – the cancer cells insidiously “removed” the CD19, becoming invisible to the lymphoma-fighting CAR T-cells, but retaining the CD20 protein.
After I went home, not thrilled about a short life expectancy that lay ahead, I put on my research hat that I use for work and started to look into monoclonal antibody “mosun” about which I had heard.
I first went to the federal website (ClinicalTrials.gov) for ongoing clinical trials and found one ongoing trial that was being sponsored by Genentech (now owned by Hoffmann-La Roche). After I reached out to them, they put me in touch with nearby Lifespan Cancer Institute in Providence, Rhode Island. Because I had had multiple prior treatments, including CAR-T therapy, I was a particularly interesting candidate.
I also inquired directly into the potential costs of the clinical trial – and found there were virtually no out-of-pocket costs to me. Because this was an approved trial with an authorized clinic, most of the costs are paid by the trial, including some scans, blood tests, extra biopsies, any hospitalizations and of course, the monoclonal antibodies themselves. Any other expenses would be covered by my insurance.
After meeting with the doctor and nurses running the trial, I was accepted and am now on my fifth out of eight cycles. Though the results are still very preliminary, they’re very promising, with over 60% of participants with NHL achieving complete response. I have had negligible side-effects, and the infusions following the rigorous protocol of monoclonal antibodies mosunetuzumab (mosun) and polatuzumab vedotin (pola) have gone smoothly. I won’t know until later if this has been totally effective in getting rid of the B-cell cancerous lymphoma until the final PET-CT scans are analyzed and hopefully the “lit-up” sites in my upper sinus area and on my liver have dimmed or disappeared. But I am feeling pretty good with no symptoms of lymphoma or evidence of it on my recent scans, and my oncologist and staff remain very optimistic.
What are the bottom-line messages from my experience?
(1) Never stop looking for the next steps in medical treatments and therapies. Even when you receive devastating results from highly experienced and competent cancer specialists that you trust completely there may be other things out there that can work for your particular situation. The medical fields in immunology and cellular sciences are changing so fast and taking place world-wide that there may be good options available although no single expert will be fully aware of them.

(2) Cancer is an incompletely understood disease and a living organism that wants to survive and reproduce, just like Darwin hypothesized for all living creatures. It learns that all these advanced chemo drugs and therapies are out to eradicate it, and just like other living organisms, it changes by transformation, modification, adaptation, and mutation. It learns and remembers what has happened in the past and adapts. It is a race between the advancements being made in the sciences and the flexibility and adaptability of lymphoma to keep surviving.
Therefore, it’s important to always “Look Beyond the Next Step.”
